MRI (magnetic resonance imaging) is the imaging modality of choice in small animal cases with vestibular disease, seizures, or other neurologic disease localized to the brain. MRI allows superior detail of the white and grey matter of the brain, as well as visualization of some of the cranial nerves, the adjacent cranium and musculature, lymph nodes, and the ears. Images are obtained without contrast initially, using a protocol of different sequences to highlight certain tissues or abnormalities (i.e. cerebrospinal fluid, hemorrhage, edema). Intravenous contrast is then administered at the end of the study to highlight certain abnormalities that disrupt the blood-brain barrier. The appearance of a lesion on the multiple different sequences and degree of contrast enhancement helps the radiologist rank differentials for the abnormalities. Below is one of the many interesting lesions we have identified on our MRI at Animal Imaging.
History
”Pinky”, a 10 year old, spayed, female Chihuahua, presented with a history of right vestibular disease that improved with prednisone and Clavamox but has not completely resolved. In addition, the patient has had generalized seizures for the past few months. Since starting phenobarbital and a course of prednisolone, no seizures have been reported. The patient was recently evaluated by an ophthalmologist and was diagnosed with optic neuritis. Phenobarbital administration had stopped one week prior to referral to Animal Imaging.
Imaging Findings
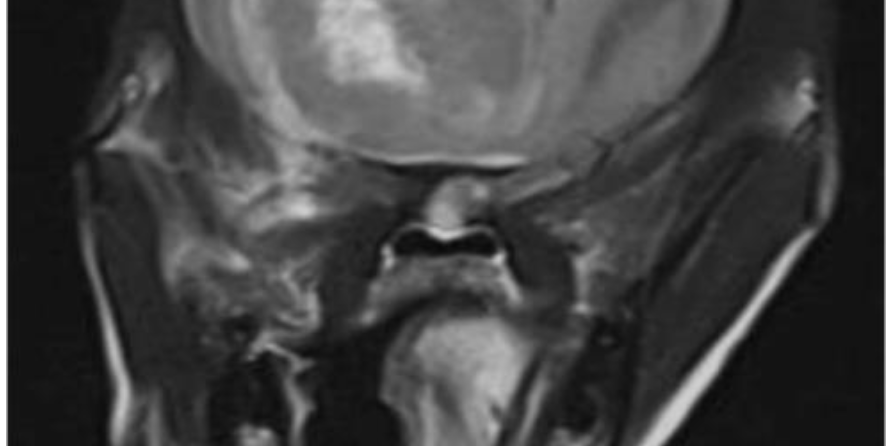
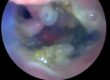
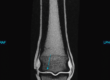
Multiplanar MR images of the brain were acquired before and after intravenous contrast. . A large heterogeneous mass was identified within the ventral aspect of the right rostral to mid calvarium, extending from the cribriform plate caudally to the level of the optic chiasm. This mass was heterogeneously contrast enhancing, with the majority of the enhancement identified along the peripheral margins of the mass. Additionally, there was evidence of hemorrhage within this mass. This mass was causing transtentorial herniation of the thalamus and midbrain with moderate secondary compression of the rostral cerebellum. No herniation of the caudal cerebellum was appreciated. Moderate-to-marked non enhancing T2/FLAIR hyperintensity was identified surrounding this mass, consistent with perilesional edema. Additionally, there was marked leftward deviation of the longitudinal fissure and compression of the left lateral ventricle.
Conclusion
Large heterogeneous intracranial, likely intra-axial, mass within the right rostral ventral cerebrum, with moderate to marked perilesional edema and transtentorial herniation. The primary differential is neoplasia, such as a glioma. While a benign etiology, such as focal granulomatous meningoencephalitis, cannot be completely excluded, is felt less likely.
Discussion
Canine glial tumors, such as astrocytomas and oligodendrogliomas, are malignant brain tumors originating from the supporting cells of the brain. Gliomas are the second most frequent type of primary brain tumor in the canine patient. These tumors occur commonly in middle to older aged patients and often occur in brachycephalic (short-nosed) breeds, such as the Boxer, Bulldog and Boston Terrier. Common signs include seizures, behavior abnormalities (i.e. aggressiveness), vestibular signs and/or visual changes and advanced imaging, such as MRI, is crucial to identifying these masses and making a diagnosis. The biologic behavior of these tumors ranges from slow growing to aggressive and gliomas are very difficult to treat. Many dogs are treated with symptomatic therapy (steroids and antiseizure medications); however, the prognosis is generally poor with an average survival of just a few months.