History and Clinical Presentation
Misty, 10-year-old quarter horse mare used for barrel racing, presented to her primary veterinarian for a chronic grade 2/5 left forelimb lameness. When blocked to palmar digital nerve anesthesia, the lameness switches to a grade 1.5/5 right forelimb lameness. Distal interphalangeal joints were injected earlier this year, and the lameness improved but never fully resolved. The horse had a previous MRI in January 2023 and was diagnosed with a collateral ligament injury to the distal interphalangeal joint at that time.
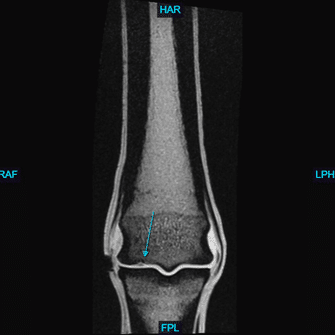
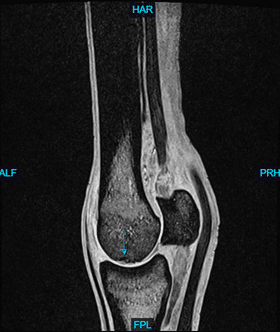
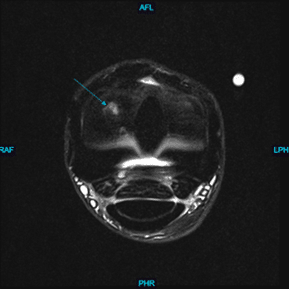
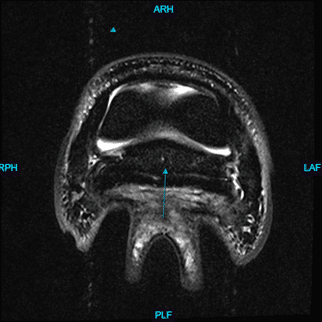
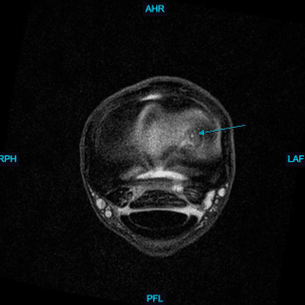
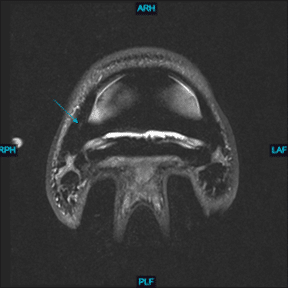
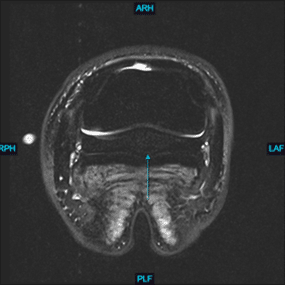
Upon presentation to Animal Imaging, the clinical picture matched that of the history from the primary veterinarian. Bilateral forefeet magnetic resonance imaging was performed and upon initial review an irregular lesion in the left distomedial subchondral bone of the third metacarpal bone was seen on the extended view of the proton density image. At this time, the Animal Imaging team recommended additional fetlock imaging to further detail the peripheral image lesion. MRI findings included:
Left Front Limb
Irregular lesion in the distomedial subchondral bone of the third metacarpal bone.
Right Front Limb
Follow Up Case Information
The primary differential for the chronic left front limb lameness was the subchondral bone defect within the left distal third metacarpal bone. Additional findings included the improved collateral ligament injury seen in the right front limb and mild bilateral navicular changes. The fetlock joints bilaterally were treated, and the lameness resolved, allowing the horse to return to primary use.
Discussion
A team-based approach for the diagnosis and treatment of lameness conditions in the horse is of paramount importance. Advanced diagnostic imaging and communication during real-time image acquisition allows for peripheral lesions to be thoroughly evaluated under one diagnostic procedure.
As equine practitioners, we understand the limitations of diagnostic analgesia. This case highlights the importance of clinical interpretation and expertise as we know from experience that 90% of palmar digital nerve diagnostic analgesia lesions occur in the foot. The remaining 10% of lameness cases that respond to diagnostic analgesia but have lesions proximal to that of the nerve block are influenced by additional factors, such as proximal diffusion of the anesthetic. This requires the lameness diagnostician to be constantly aware of peripheral lesions that may be present and be contributing to the primary lameness.
A team-based approach towards lameness diagnoses including advanced imaging ultimately leads to improved care for the horses and clients.